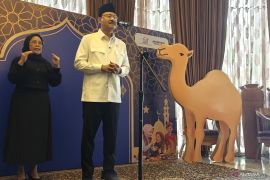
Speaking at the 1st Indonesia Healthcare Anti-Fraud Forum (INAHAFF) held here on Wednesday, he explained that over the past two decades, JKN has reduced nearly 70 percent of public healthcare expenses and covers premiums for around 96 million underprivileged Indonesians.
Therefore, he stressed that any fraud occurring in JKN constitutes a moral and constitutional violation.
"One instance of healthcare service fraud can cause an entire family to lose the opportunity to escape poverty," he said.
Iskandar said that INAHAFF offered an opportunity to learn innovative anti-fraud strategies from countries such as Egypt, China, and Malaysia. Approaches include claim analysis centers, specialized health anti-fraud units, and law enforcement initiatives.
The common goal is building a comprehensive framework for early detection, prevention, and coordinated action.
He outlined five potential sources of fraud, which are hospitals or clinics inflating bills, doctors manipulating diagnoses or prolonging illness, state health insurer BPJS Kesehatan staff failing to verify claims properly, participants falsifying identities or documents, and policymakers creating regulations benefiting certain parties.
"Every rupiah of public and state funds must return as quality healthcare services and serve as a real foundation for community empowerment," he emphasized.
To strengthen anti-fraud measures, the minister proposed enhancing regional capacity involving numerous parties.
"Concrete steps include strengthening regional capacity to prevent fraud. Regional anti-fraud forums involving the community, local governments, hospitals, clinics, BPJS Kesehatan, and law enforcement are needed to cultivate an anti-fraud ecosystem," he said.
Related news: Govt reaffirms BPJS health for all people, regardless of social class
Related news: Indonesia ensures health insurance for 96.8 million people
Translator: Mecca, Kenzu
Editor: Arie Novarina
Copyright © ANTARA 2025